Mast Cell Activation Syndrome (MCAS) - Much More Than Just A Histamine Issue
How I've learned to manage MCAS - approaches to treatment, the challenges with diagnosis, and how MCAS differs from and overlaps with histamine intolerance
Mast Cell Activation Syndrome (MCAS) is one of the most common yet least understood disorders plaguing people with chronic health conditions.
It is thought by experts to affect 1 in 6 people, or 17% of the population, and it is a common comorbidity of nearly every prevalent ailment faced by those with chronic illness.
On the one hand, mast cells are the unsung heroes of the immune system. They are the first line of defense scanning for any threat to your body - physical or emotional. Mast cells serve as a communication bridge between the immune system and the nervous system, telling your body how to react to its environment.
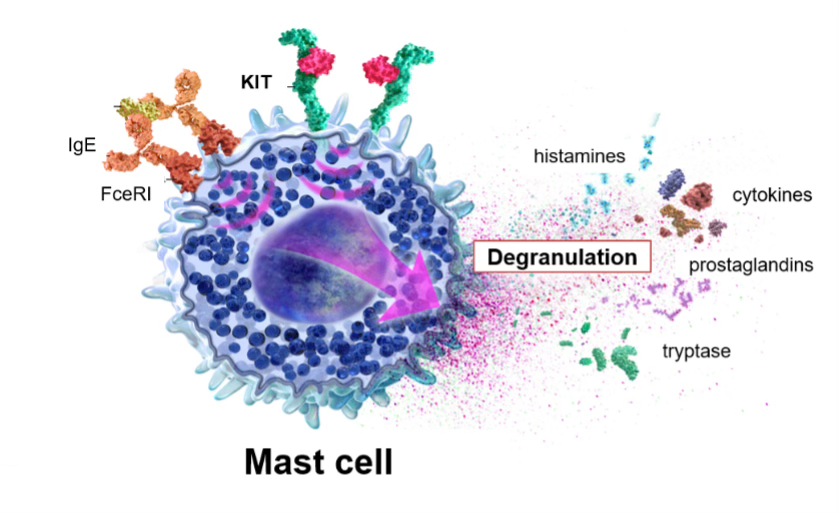
However, in the face of insurmountable stress - again, physical or emotional - mast cells begin to act erratically, degranulating on a dime and releasing a wide array of chemical mediators, causing a variety of widespread and commonly misunderstood symptoms.
This often looks like a woman who has faced a major viral or bacterial illness, or a major stressor like college or a divorce, or just had a baby, and begins to experience several new and confusing symptoms including fatigue, hives, brain fog, and "food sensitivities," resulting in endless referrals only to be told her labs are “normal.”
MCAS is a condition where the immune system becomes its own worst enemy - subtle, complex, and routinely misunderstood.
First, what is MCAS?
Mast Cell Activation Syndrome (MCAS) is an immune system disorder.
Your immune system has cells called mast cells. They act as the "alarm system" of the immune system that release hundreds of chemicals (including histamine) when they detect danger (like stress, an allergy trigger, or an infection). Mast cells act as messengers at the crossroads of the immune and nervous systems, translating danger into sensation and response.
In MCAS, mast cells go haywire, and release too many chemicals too often - even when there's no real danger. This causes symptoms like hives, flushing, brain fog, racing heart, systemic inflammation, gastrointestinal distress, and more.
Histamine is not the only mediator released by mast cells.
There is a lot of talk in the health and wellness world about histamine - and for good reason. An overload of histamine can cause a variety of health and psychiatric symptoms which are largely overlooked by the medical industry. From anxiety and depression to bloating, fatigue, and digestive issues, histamine is involved in many chronic “mystery” conditions. Unfortunately, most doctors - even allergists - are completely uninformed about the causes and solutions for an overload of histamine, including MCAS.
However, for many - histamine is just the tip of the iceberg.
And for many more - histamine is not the only, or even the primary issue with MCAS.
Mast cells can be triggered by anything perceived as a stressor to the body - physical or emotional stress, heat/temperature changes, infections, allergies, food, alcohol, and medications, to name just a few.
In response to this stressor, mast cells degranulate and release hundreds of chemical mediators. Histamine gets a lot of attention because it tends to be the most recognizable in terms of symptoms, and one of the most dangerous because it can cause anaphylaxis. However, histamine is just one of the many inflammatory chemical mediators released by mast cells that causes problematic symptoms.
Even people even who are aware of MCAS often don’t realize they or their children are dealing with it - either because they don’t have the stereotypical histamine issues, or they don’t think their illness is as severe as it “should be” with MCAS, or some other issue that comes down to simply misunderstanding MCAS. And unfortunately, this means many people will suffer moderately, playing whack-a-mole with their symptoms - until their body becomes completely overwhelmed and slams into a wall, multiplying their symptoms.
Mast Cell Mediators
Mast cells release hundreds of chemical mediators such as inflammatory cytokines, leukotrienes, and prostaglandins. These substances contribute to a wide range of symptoms, including widespread tissue inflammation, increased vascular permeability (which can lead to POTS and other dysautonomia symptoms), and smooth muscle contractions that may cause intermittent or persistent pain - often difficult to diagnose. The effects of these and other chemical mediators can extend even further, influencing multiple body systems.
Some of the chemical mediators released by mast cells and their potential effects include:
Histamine: Skin flushing, itching, digestive disturbances, low blood pressure
Prostaglandins: Skin redness, bone pain, cognitive difficulties, muscle cramps
Serotonin: Nervousness, agitation, confusion, rapid/abnormal heart rate, high blood pressure
Leukotrienes: Difficulty breathing, vascular permeability
Tryptase: Bone density loss, skin abnormalities
Interleukins: Chronic fatigue, weight loss, swollen lymph nodes
Heparin: Bone density loss, clotting or bleeding issues
Tumor Necrosis Factor-a: Tiredness, headaches, body aches
Symptoms are extremely diverse, wide ranging, fluctuating, and seemingly disconnected.
Unfortunately, many patients with MCAS are completely dismissed by most doctors as having a psychosomatic disorder because anxiety and depression are often related symptoms. Compounding the issue is that MCAS can actually cause and worsen a number of chronic conditions that have been identified within the medical system as isolated conditions, instead of multi-systemic inflammatory immune issues, leading to misdiagnosis. These conditions include POTS and dysautonomia, hypermobility and EDS, fibromyalgia, chronic fatigue syndrome, autoimmune disorders, IBS/IBD, and other inflammatory and immune conditions.
Symptoms that can be attributed to MCAS include:
Psychological: Intense anxiety and depression, mood swings, panic attacks
Neurological: Headaches, debilitating fatigue, insomnia and sleep disturbances, severe pain, numbness and tingling, paralysis, pseudoseizures, ringing in the ears, difficulties with equilibrium and balance
Cognitive Difficulties: Brain fog, decreased focus, memory, and concentration
Respiratory: Shortness of breath, air hunger, wheezing, difficulty breathing
Dermatological: Skin rashes, hives, flushing, itching,
Immunological: Sore throat, swollen lymph glands
Digestive: Nausea, vomiting, heartburn/indigestion, interstitial cystitis, symptoms commonly associated with IBS/IBD like abdominal pain, diarrhea, constipation, bloating, gas
Cardiovascular: Low blood pressure, rapid heart rate, fainting, and lightheadedness
Increased Sensitivity: light, touch, sound, smells, foods, chemicals, and electromagnetic frequencies (EMF)
Chronic, Systemic Inflammation
MCAS and Histamine Intolerance
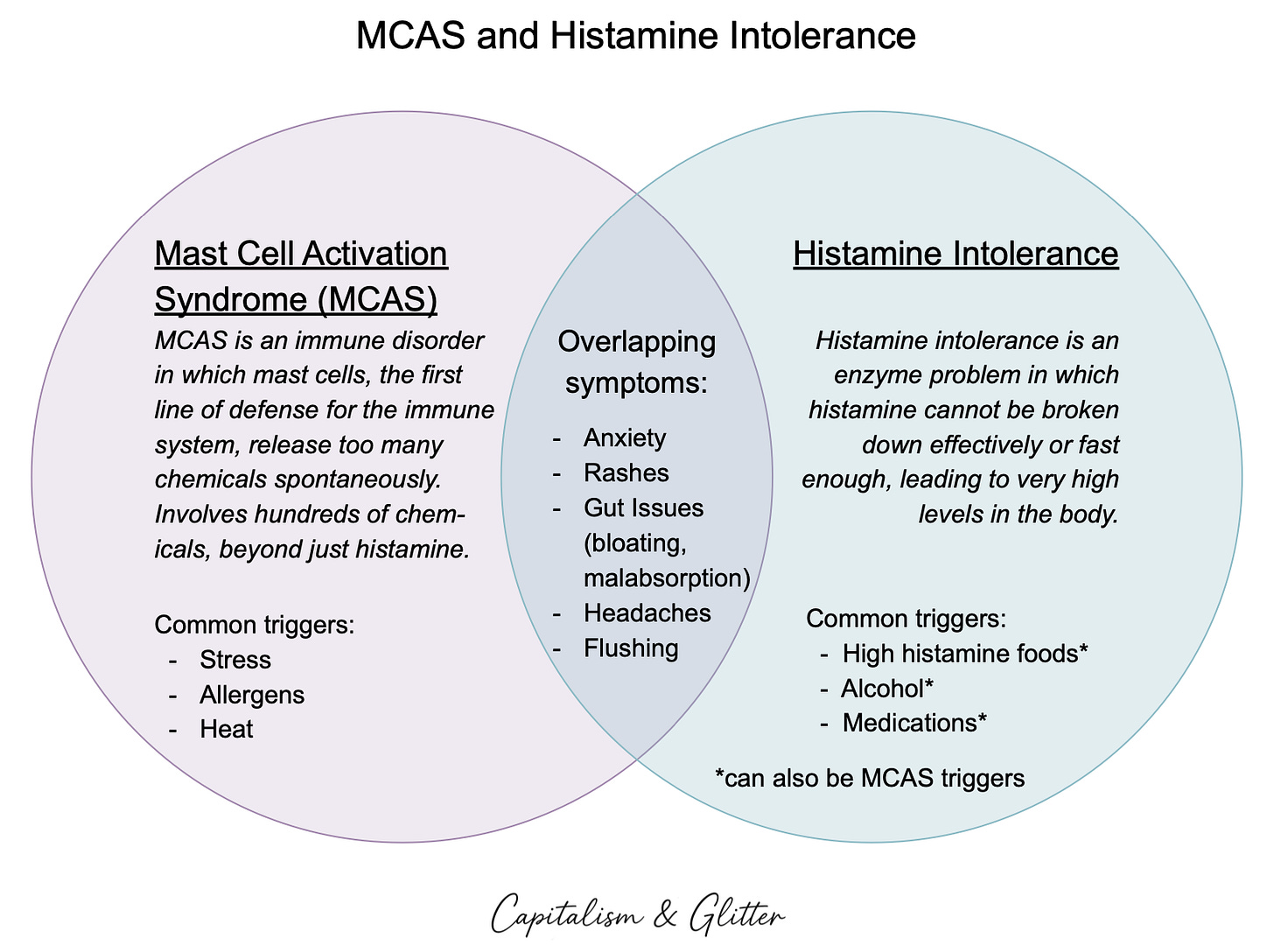
There are two predominant causes of an overload of histamine in the body, which have overlapping symptoms, but different etiologies and somewhat differing strategies and solutions to support - Mast Cell Activation Syndrome (MCAS) and Histamine Intolerance. MCAS is much more common, is often confused with histamine intolerance, and includes hundreds of other inflammatory chemical mediators beyond just histamine, as previously discussed.
While MCAS is an immune system disorder, histamine intolerance is an enzyme issue.
Histamine is a natural chemical your body makes that is crucial for various biological processes. Many people are familiar with its role in allergic reactions, but it’s also involved in digestion, inflammation, and circadian rhythm (sleep-wake cycles). Histamine is also found in certain foods (like aged cheese, beer and wine, and fermented stuff).
With histamine intolerance, your body can’t break down histamine effectively or fast enough, usually because of a problem with the DAO (diamine oxidase) enzyme. Histamine then builds up and causes allergy-like symptoms, including headaches, runny nose, itchy skin, etc.
While MCAS is present in 17% of the population, histamine intolerance is estimated to be present in up to 3% of the population.
How are they similar?
Both MCAS and histamine intolerance cause symptoms resulting from too much histamine in the body. That’s why they often look alike. Things like anxiety, headaches, flushing, rashes, and stomach issues can happen in both MCAS and histamine intolerance. People with either condition often react poorly to histamine-rich foods.
Both MCAS and histamine intolerance can cause dangerous levels of histamine in the body that result in anaphylaxis - a life threatening allergic reaction that can affect the heart, lungs, skin, and more.
How are they different?
While both conditions can lead to an overload of histamine in the body, the causes are different - and therefore the potential treatment options differ.
Mast cells cause an overload of histamine as well as hundreds of other chemical mediators that are problematic in large quantities - including prostaglandins, inflammatory cytokines, etc.
MCAS triggers include:
Stress/Trauma
Heat
Allergies
Infections
Food
Alcohol
Medications
Histamine intolerance occurs when you can’t break down the overload of histamine properly and rid it from the body. Histamine intolerance usually occurs due to a functional deficit of the DAO enzyme. Histamine intolerance can occur alongside MCAS and can be exacerbated by mast cells erratic release of excess histamine, as an excess of histamine can overwhelm the amount of DAO enzyme available.
Histamine intolerance triggers include:
Foods including fermented foods, processed foods, aged foods, some fruits
Alcohol
Medications
Chances are, if you are dealing with this overlap of symptoms, you are much more likely to be dealing with MCAS than histamine intolerance - though a not insignificant percentage of the population is dealing with both, and MCAS can cause temporary histamine intolerance by overwhelming the DAO enzyme availability.
The Role of the Liver
The liver plays a key role in clearing histamine from the body. Impaired liver function can also reduce the body’s ability to clear histamine, and it can occur in both MCAS and histamine intolerance. The liver’s ability to detox histamine is reliant on several other pathways, including methylation and sulfation; sufficient nutrients, including magnesium and several B vitamins; and open drainage pathways, including lymphatics and excretion of waste.
Read on for more about the issues with testing and diagnosis as well as treatment options.